News
22.12.2022
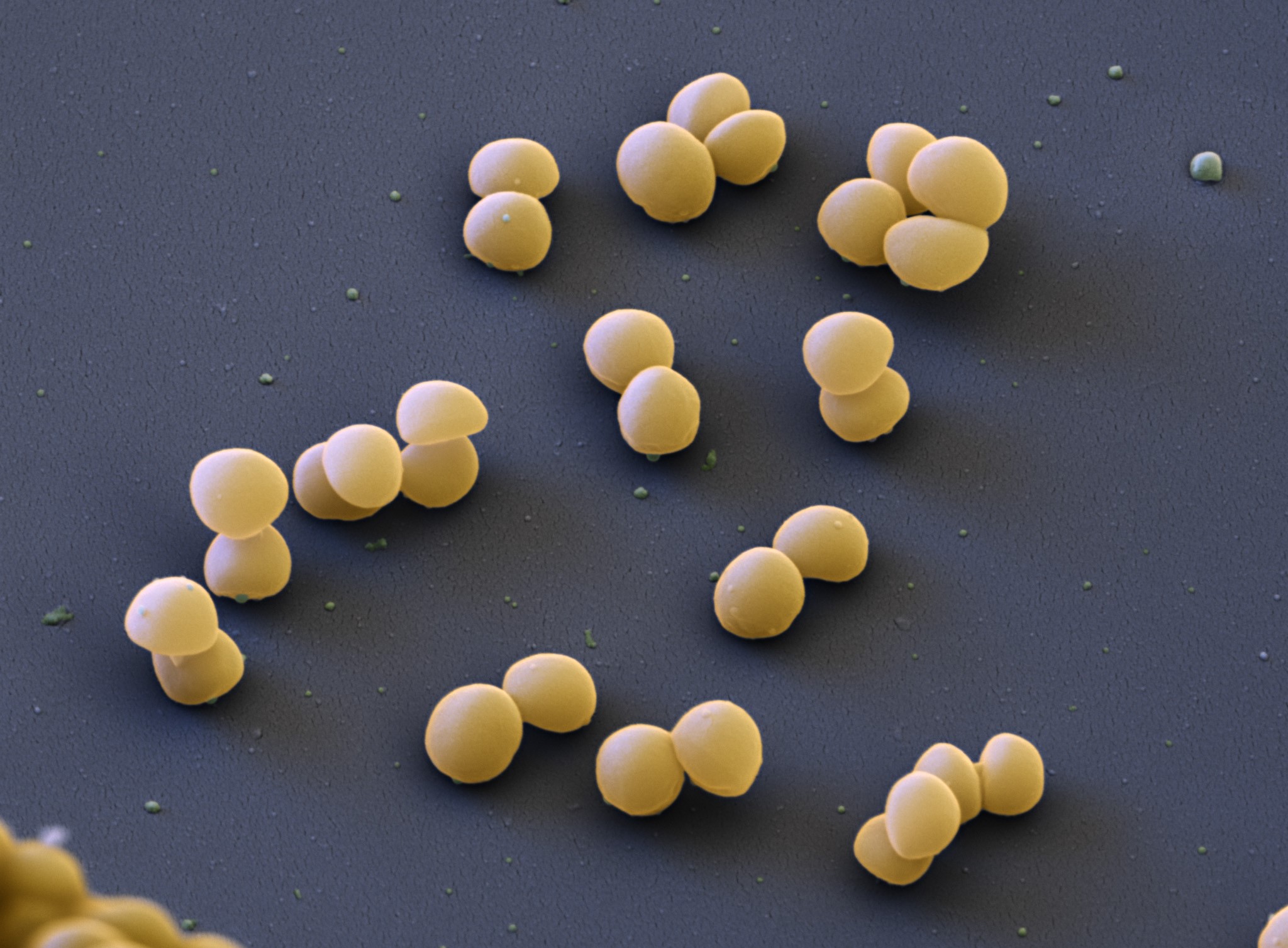
Finding a peptide drug against MRSA
Drug-resistant Staphylococcus aureus strains have become a major global burden due to their high morbidity. Infections are usually treated with broad-spectrum antibiotics that not only kill the pathogen but also many beneficial commensal bacteria. It would therefore be desirable to develop an agent that targets only S. aureus. The study “From a Hsp90 – binding protein to a peptide drug” in microLife describes the identification of such a drug. Aparna Viswanathan Ammanath and Friedrich Götz explain for the #FEMSmicroBlog how this approach could help us tackle one of the major global challenges. #FascinatingMicrobes
About resistant Staphylococcus aureus
Over the past 30 years, infections have become difficult to treat due to the increasing prevalence of antibiotic resistance mechanisms. Of particular concern are methicillin-resistant S. aureus (MRSA) and multidrug-resistant S. aureus (MDRSA) strains that are spreading worldwide.
Multiple studies in hospitals across the United States and European Union have shown that MRSA is the most common cause of skin and soft tissue infections. MRSA colonization is associated with subsequent infection and increased morbidity and mortality.
Consequently, the economic burden from infections caused by these strains has dramatically increased in both the USA and the European Union/European Economic Area (EU/EEA). To meet this challenge, detailed research into the factors responsible for the spread and epidemiology of MRSA and MDRSA is necessary. If we better understand these factors, we can take specific measures to reduce the spread. The study “From a Hsp90 – binding protein to a peptide drug” in microLife presents a non-antibioticbased approach to reduce the pathogenicity and possibly the spread of MRSA and MDRSA.
Identifying surface targets for antivirulence drugs
Almost all bacteria contain bacterial lipoproteins (Lpp) on their cell surface. In Grampositive bacteria, these proteins are anchored to the cytoplasmic membrane and protrude outwards. Here, they uptake nutrients and interact with host cells.
Lpl lipoproteins belong to a class of Lpp, of which the membrane-anchored lipoprotein Lpl1 of S. aureus is a model protein. Upon infection of the host, Lpl1 binds to human Hsp90. This interaction triggers a number of responses in S. aureus such as the increased invasion of epithelial cells, increased formation of filamentous actin (F-actin) and increased virulence.
Hence, the study speculated that blocking this essential interaction could reduce the virulence of S. aureus. In an attempt to identify the Lpl1 domain that interacts with Hsp90, peptides were synthesized that derived from the Lpl1 protein. Two of these peptides, L13 and L15, indeed bound to Hsp90 and Lpl1, while the binding to the parent protein Lpl1 was rather surprising.
When epithelial cells were infected with S. aureus, adding L13 and L15 decreased bacterial invasion, F-actin formation and virulence. It was assumed that the binding of L15 and L13 to both the bacterial ligand Lpl and the host cell receptor Hsp90 prevents the activation of Hsp90.
Potentially stopping the global S. aureus spread
While L13 and L15 are unable to prevent S. aureus from growing, treating animals with the peptides in an infection model significantly reduced the pathogenicity of S. aureus.
In this respect, L15 and L13 cannot be considered antibiotics in the true sense of the word but anti-virulence compounds.
Interestingly, the genes for the biosynthesis of the Lpl proteins are present in all S. aureus strains investigated so far. The genes are clustered in a pathogenicity island which appears to be unique in S. aureus and some other pathogenic staphylococcal species. Therefore, the effects of L13 and L15 are limited to these species.
Epidemic and globally spreading S. aureus strains have a particularly high number of lpl orthologous genes. It is tempting to speculate that this gene cluster contributes to the rapid spreading of MRSA and MDRSA. Therefore, the two novel peptide drugs L13 and L15 could be employed to not only decrease S. aureus pathogenicity but also limit the spread of the epidemic strains.
Read the article “From a Hsp90 – binding protein to a peptide drug” by Ammanath et al. (2022).
About the authors:
Aparna Viswanathan Ammanath did her master’s studies at the Amrita Centre for Nanosciences and Molecular Medicine, Amrita University, Kerala, India. She is finishing her PhD in Microbial Genetics at the University Tübingen. Aparna studies mechanisms of new antimicrobial agents and works on new concepts for the development of targeted anti-infectives.
Prof. Dr. Friedrich Götz holds a Senior-professorship at the University Tübingen, Interfaculty Institute of Microbiology and Infection Medicine (IMIT) and is a member of the Cluster of Excellence 2124 ‘Controlling Microbes to Fight Infections’ (CMFI). His research interest includes the physiology of staphylococci and their interactions with humans.
(Source: FEMS Microbiology Blog)